According to the U.S. Department of Health and Human Services, one in four babies is now delivered by Cesarean — the highest level ever reported, and over 10 percent higher than in countries with similar demographics. But a new consumer booklet, What Every Pregnant Woman Needs to Know about Cesarean Section, from the Manhattan-based Maternity Center Association (MCA), warns that C-sections are associated with significant short- and long-term physical and emotional health risks for both mother and baby. Concerned about the potentially misleading and incomplete information on Cesareans provided by individual studies and media reports, MCA reviewed over 300 research studies on various birthing options. “We wanted to determine the true risks associated with Cesareans, to ensure that women have the best information for making informed decisions,” says Maureen Corry, MCA’s executive director. The MCA review compared the risks and benefits of Cesareans with those of vaginal birth.
Cesarean risks for mothers MCA found that women who undergo Cesareans experience more severe and longer-lasting pain than with vaginal birth. Pain was the leading postpartum health concern in the first two months after Cesarean for over 80 percent of women in a recent national survey. Dr. Eugene Declercq, co-author of the resulting report, Listening to Mothers, adds, “Even six months after Cesarean delivery, pain continued to be a problem for one in 14 women who had a Cesarean. Yet many women fear vaginal birth because they worry about the pain.” The survey also revealed that women who had Cesareans were more likely to experience bladder and bowel difficulties, headaches and backaches. Women who have Cesareans are also more likely to be re-admitted to the hospital in the weeks after birth and are much more likely to have an infected uterus than those who deliver vaginally. Between one and nine out of every 1,000 women who give birth by Cesarean are at added risk for an emergency hysterectomy in the early weeks after giving birth.
Cesarean risks for babies A baby born by Cesarean may suffer accidental cuts (usually minor) during the surgery. MCA estimates that this occurs in between one and nine of every 100 Cesareans. Due to the pain, lengthy recovery period, and risk of infection and complications, a mother who has had a Cesarean has less early contact and may have an early negative reaction to her baby, affecting maternal bonding. Cesarean-born babies are less likely to be breastfed, missing important health benefits, and they have a high risk of early respiratory problems and lifelong asthma.
Cesarean risks for future pregnancies Women who undergo Cesareans (versus vaginal birth) have a very high risk of later infertility. For those who do conceive again, between one and nine out of every 1,000 have an increased risk of ectopic pregnancy, placental issues (placenta previa, placenta accrete or placental abruption) or a ruptured uterus. A baby who develops in a uterus with a Cesarean scar appears to have a moderate risk (one to nine of every 1,000) of dying before or shortly after birth.
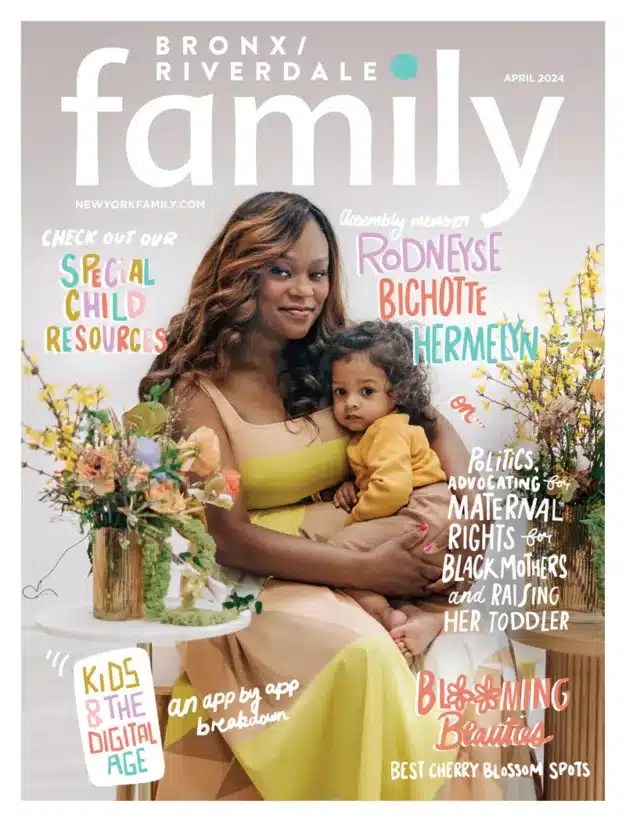
Concerns for older mothers These findings are particularly important for older women who have postponed childbearing. “Pregnant women over 35 are often automatically classified ‘high risk’ and targeted for Cesareans,” says Dr. Declercq. “Instead, we should look at the medical risk factors of each individual woman. Age alone is not a risk.” If fertility drugs have resulted in a woman carrying twins, triplets or more, physicians typically recommend a Cesarean. “Fewer and fewer doctors have the skills to deliver multiple births vaginally,” says Dr. Declercq. “As those skills are increasingly lost, this will become a self-perpetuating cycle.” Older women who have invested a lot emotionally and financially trying to conceive may be urged to undergo a Cesarean to minimize risks to the baby. “These mothers may feel there is no room for error or uncertainty,” observes Dr. Andrei Rebarber, maternal fetal medicine specialist at NYU School of Medicine. While he acknowledges that a Cesarean gives more control over the fetus, Dr. Rebarber advises women to evaluate all options carefully before making a decision. Tonya Jamois, president of the International Cesarean Awareness Network (ICAN) cautions, “Doctors have their own sets of constraints — their schedule, their liability — that may bias their recommendations. Women need to clearly understand the risks and benefits of both Cesarean and vaginal birth from an unbiased point of view.”
Cesarean rate increasing In 1970, one woman in 20 gave birth by Cesarean. Today, nearly six in 20 do so. The Centers for Disease Control (CDC) have expressed concern about the growing Cesarean rate among healthy, low-risk women. The U.S. Department of Health & Human Services advocates reducing Cesareans for low-risk women to less than 15 percent by the year 2010. The World Health Organization estimates that half of all Cesareans performed in the U.S. are unnecessary. There is no debate that Cesareans are absolutely necessary in the presence of urgent medical concerns. Cesareans can save lives or prevent serious injury to mother and baby if the mother is hemorrhaging or the baby’s oxygen supply is seriously compromised.
VBACs declining The “once a Cesarean, always a Cesarean” debate continues. The rate of vaginal births after Cesarean (VBAC) has plummeted 55 percent since 1996. A 1999 American College of Obstetricians and Gynecologists (ACOG) bulletin urged practitioners to offer VBACS only where facilities, anesthesia and nursing personnel are “immediately available” to perform emergency Cesareans. As a result, many smaller hospitals without 24/7 surgical staffing have adopted a “no VBAC” policy. ICAN provides advice for women faced with forced Cesareans due to such policies. (see Resources).
“Defensive medicine” Medical, legal, social and financial factors contribute to the increasing Cesarean rate. “Lawyers tell OBs that few lawsuits occur if you perform a Cesarean too soon,” says Dr. Rebarber. “Lawsuits occur when you perform a Cesarean too late or not at all.” For New Yorkers, the legal climate in obstetrics led to the closing of the only freestanding birth center in Manhattan. Midwives, as well as MDs, are forced at times to practice defensively, resulting in more interventions. Physicians increasingly use medical interventions that can lead to Cesarean. “The long term trend has been that practices that were developed and appropriately applied to high-risk mothers are slowly but surely being used with more and more mothers, based not on actual medical risk but on potential medical risk,” says Dr. Declercq. “For example, fetal monitoring is beneficial for mothers in a high-risk pregnancy, but it has very little or negligible benefit for low-risk mothers. Yet it’s used in about 93 percent of all pregnancies.” He explains that irregularities sometimes appear on monitoring strips even when nothing is wrong with the baby. “A Cesarean is regularly done if there’s any question about the results,” Dr. Declercq says, “because it’s almost impossible to explain to a courtroom jury in a case with a bad outcome that an irregularity on a fetal monitoring strip was not a definitive sign of a problem.” Dr. Rebarber adds that when labor isn’t progressing, some doctors still use the 1960s Friedman Curve to decide when to induce labor or perform a Cesarean. “Newer criteria indicate that women should be given more time for labor to progress before jumping to a C-section,” says Dr. Rebarber. “If both doctor and patient know these new criteria and are prepared for longer labor, often a Cesarean can be avoided.”
Elective Cesareans vs. vaginal birth Women play a role in the increasing Cesarean rate as well. Fear of vaginal birth pain or concerns about the risk of later-life problems with incontinence or sexual dysfunction lead some women to request Cesareans. However, it is not vaginal delivery itself, but overused medical practices during vaginal birth that cause these problems. These problematic medical practices include episiotomy, delivering while lying on the back, caregiver-directed pushing (versus allowing the woman to follow her own natural instincts in pushing), and pressing on the woman’s abdomen or perineum. “Ask caregivers about their use of these practices and clearly communicate your own preferences,” Corry advises.
Labor support “If we could give one gift to every pregnant woman, we’d provide her with a doula,” says Corry. A doula is a trained labor companion who provides physical and emotional support. MCA reports that women who receive continuous professional labor support are significantly less likely to have a Cesarean, use pain medications, or be dissatisfied with their birth experience.
Making an informed decision Corry spells out four critical steps for women to help ensure a positive birth experience: • understand your choices and rights • choose a caregiver and birth setting that will support what you want (see: Questions to Ask) • develop good communications with your caregiver and be prepared for possible last-minute decision-making during labor, and • arrange for labor support from a doula or other professional. “The way a woman gives birth can impact her and her family in ways she might not expect,” says Corry. “A safe and satisfying childbirth experience provides an excellent foundation for taking on the new responsibilities of parenthood.”
Sidebars: Resources: • Maternity Center Association: nonprofit founded in 1918 to promote safe, effective, and satisfying maternity care for all women and their families through research, education, and advocacy. www.maternitywise.org/mca • International Cesarean Awareness Network (ICAN): nonprofit founded in 1982 to improve maternal-child health by preventing unnecessary Cesareans through education, providing support for Cesarean recovery, and promoting Vaginal Birth After Cesarean (VBAC). www.ican-online.org • Advice on addressing “no VBAC” policies: www.ican-online.org/resources/white_papers/wp_denyvbac.htm • Doulas and labor support professionals at: Association of Labor Assistants & Childbirth Educators: www.alace.org Doulas of North America:www.dona.org/FindingADoula.html
Publications: • What Every Pregnant Woman Needs to Know about Cesarean Section: www.maternitywise.org/pdfs/cesareanbooklet.pdf • Listening to Mothers: Report of the First National U.S. Survey of Women’s Childbearing Experiences: www.maternitywise.org/pdfs/LtMreport.pdf
Questions to ask of a potential obstetrical caregiver (from MCA publication: What Every Pregnant Woman Needs to Know about Cesarean Section) 1. How do you feel about epidurals? 2. How do you feel about labor induction (starting labor artificially)? 3. How often do you cut episiotomies? 4. What are my options if my labor slows down or stalls? 5. During labor, can I have my baby monitored with a hand-held device or occasional electronic fetal monitoring (EFM) rather than continuous EFM? 6. What are your rates for Cesarean section, assisted vaginal birth and episiotomy? 7. What is your epidural rate? “Choosing a caregiver and a birth setting with low rates of labor and birth interventions may be the single most important way for you to avoid the risks of unnecessary interventions, including Cesarean delivery.”
————————————————————————————————— Coming soon to a hospital near you? A hospital group in Massachusetts has joined six states in disallowing vaginal deliveries after a Cesarean section (VBAC). Although The New England Journal of Medicine gives a less than 1 percent chance of uterine rupture in VBACs, the president of the hospital group said risk and fear of liability led to the decision. Some hospitals in NY State (but not in NYC) also do not allow VBACs.
Tell us about your experience! Have you had a VBAC? Would you consider having one? Email us at: [email protected] Fax us at: (212) 689-4958 Write us at: Editorial Department, Family Communications, 9 East 38th Street, 4th floor, New York, N.Y. 10016