It’s important to know the difference between keeping our kids clean and keeping them sterile.
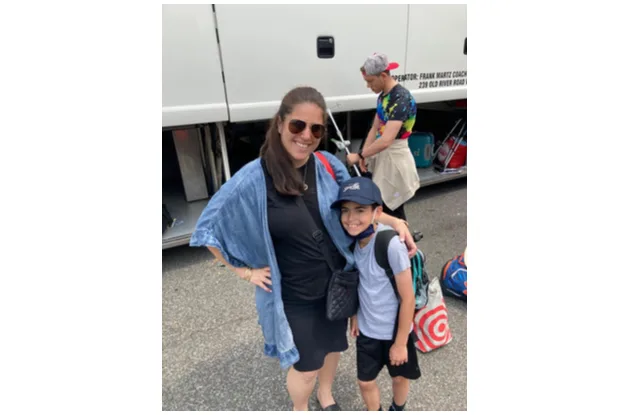
In the wake of the recent news that the FDA has ordered many antibacterial soaps off the shelves, I have a surprising call to action for parents: Sit your toddlers on the floor, let the dog lick their faces, and use plain soap and water to later wash your toddler’s hands. A move away from antibacterial products isn’t a call to avoid dirt—it’s a reminder that what lives in mess is often our friend.
The FDA’s concern is that in our effort to rid our lives of microbes, we are doing two things that will harm us. First, we are wiping out the bacteria that actually help us in countless ways, from digesting food to supporting our immune system in avoiding disease. The other concern is that we are contributing to the growing threat of bacteria that are resistant to medications, the so-called “superbugs.”
The Role Microbes Play
To really understand the thinking behind the FDA decision, it’s important to understand the countless microbes that surround us and the billions that inhabit our bodies. We cannot and should not live without them.
As referenced in Ed Yong’s book, I Contain Multitudes, when it comes to microbes in our environment, diversity is best. We have more bacteria in our intestines than there are stars in the sky, yet a small fraction of those—fewer than 100 species—actually cause infection. The rest do not cause disease, and many actually work to protect our health. These include those bacteria that synthesize Vitamin K to protect us from bleeding to death.
At birth, legions of microorganisms “set up shop” in and on the newborn, aiding digestion and keep harmful microbes away. There is a temporary suppression of the infant’s immune system that allows for this establishment of microorganisms. Sugars in human milk actually nourish the bacteria that live in the baby’s intestine. Keeping the bacteria healthy keeps the infant healthy. Research even shows that an antibody in human milk (Secretory Immunoglobulin A or SIgA) assists in setting up the healthier environment in the baby’s intestine, which is associated with less diarrheal illness in the infant and a reduction of inflammatory bowel disease and other chronic diseases later in life.
In our industrialized society with its anti-bacterial soaps, lotions, and cleansers we have almost “sterilized” our microbe environment, leaving fewer “good” bacteria to fight the “bad” bacteria. However, it is frequent challenges to our immune system from everyday bacteria that keep our army of good microbes in fighting shape for the more dangerous threats to our health.
In fact, you may be surprised to know that the licks of dogs contain microbes that are thought to strengthen the immune system of children, which may relate to a decrease in the frequency of asthma and other allergies.
None of this, however, is to discount the danger of some bacteria and the millions of lives that have been saved by hygienic practices and the judicious use of antibiotics. Hand washing with plain soap and water for 20 seconds or cleansing with an alcohol-based sanitizer for 15 seconds remains the most effective way to prevent infection.
The Rise of Antibiotic-Resistant Bacteria
The other issue that the FDA is addressing through this action is the rise of bacteria that are now resistant to treatments like antibiotics. Antibiotic resistance is the ability of a microorganism to resist the effects of an antibiotic to which it was once sensitive. The unnecessary and broad prescribing of antibiotics has led to this increase in resistance and serious infections which are becoming more deadly. Each year, there are more than 700,000 deaths worldwide due to antibiotic resistance with 10 million per year predicted to occur by the year 2050.
One example of an increasingly antibiotic resistant bacterium is Clostridium Difficile (or “C.Diff”), which causes more than 200,000 cases of a serious and often fatal infection of the colon in the US each year. C.Diff can make your grandparent’s simple hospital stay morph into a life-threatening contagious illness. This can occur because of the altered balance of “good vs. bad” bacteria in the intestines and the overgrowth of the toxic C.Diff bacteria. Complications can occur even when antibiotics are used appropriately, but we need to focus on decreasing unnecessary prescribing, such as for patients with viral conditions like the common cold. Antibiotics don’t treat viral infections. Never. Ever.
While the main cause of this increasing resistance is the misuse of antibiotics, this is part of a much larger issue. We are also contributing to resistance when we overuse anti-bacterial products. You can think of the issue of antibiotic resistance as an arms race between humans and the bad bacteria. Our efforts to blindly avoid bacteria are only tipping this arms race in the favor of the bad bacteria.
So what can you do? Remember that bacteria aren’t the enemy and we need a diverse balance of good and bad bacteria in and on our bodies and in our environments. Help your children build up their own defense to the bad bacteria. Let the dog lick your child. Allow your child to play on the floor. Don’t follow her around with anti-bacterial wipes. And only take antibiotics when it is appropriate. Remember that we can be clean without trying to be sterile. And we’ll all be much better off.